Real-Time Eligibility Inquiry
Overview
Use Revenue Performance Real-Time Eligibility Inquiry to check eligibility based on each payer's eligibility search requirements. In addition, you can create batch requests for multiple patients and payers.
Step-by-Step
Here is an example of a Real-Time Eligibility Inquiry:
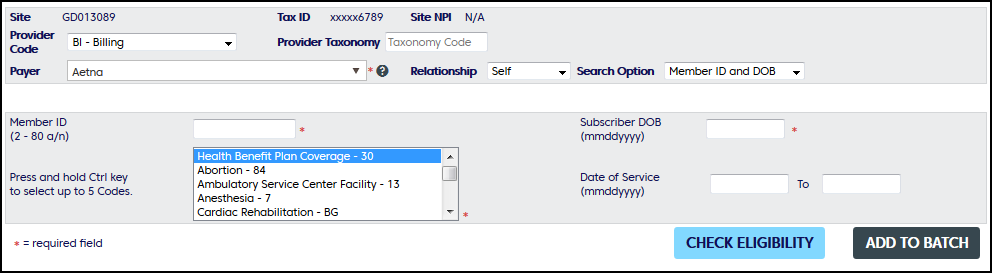
Top Section: Use the drop down lists to select the Site and NPI search options. You can choose to enter a Taxonomy and Provider Code but it is optional, as most payers do not require this information. If you wish to enter a taxonomy code, start typing in the auto-complete Taxonomy Code box and matched codes will automatically display for you to choose. The Payer field is waiting on you to start typing either the payer name or payer id or select from your favorite payer list. To create a list of favorite payers, select a payer and click on the 'star' next to the payer name. Repeat to add as many payers as you want. To display the list of favorite payers, select the dropdown arrow. The favorite payers will be listed first. To remove a favorite, select the dropdown arrow to display your favorite payers and click the 'star' to remove it from your favorite list.
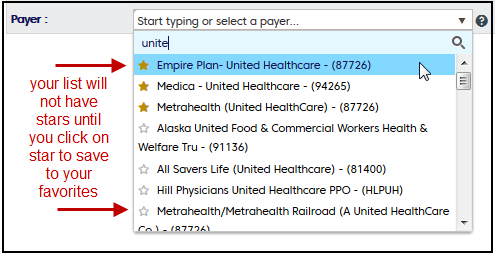
Example: Payer selection list
Next Section: Shows the patient search option criteria for your selected payer. Required fields are marked with an astrik.
Click Check Eligibility if you are only doing one request. Use Add to Batch for multiple requests.
Add to Batch: This is used to start a batch of multiple inquiries. You may submit up to 50 inquiries at one time.
Service Type Code: The options offered are based on the eligibility requirements of each payer.
- For some payers, you will have the option to select one or more Service Type Codes, including Health Plan Benefit Coverage - 30. To select multiple Service Type Codes, hold the CTRL key and select additional codes. If Health Plan Benefit Coverage - 30 is not offered, we send it by default.
- For some payers, you will not have the option to select any Service Type Codes. For those payers, Health Plan Benefit Coverage - 30 is sent by default.