CCI and MNC
Overview
Correct Coding Initiative (CCI) and Medical Necessity (MNC) are a system processes that check claims for valid combinations of clinical codes and for pre-defined criteria for being medically necessary.
This help page is a guide to the new information offered in the claim detail page for CCI and MNC results.
What are CCI and MN?
Correct Coding: This function validates: that codes make sense for the patient, that they belong together. It also performs other "logic" coding validation.
It also identifies national correct coding methodologies to control improper coding that would cause improper payment. CCI policies are based on coding conventions defined in the AMA CPT manual and from national and local policies.
Medical Necessity: This function validates medical necessity against a number of national and local policies.
CCI and MNC Status Options:
Passed: Claim passed CCI and MNC validation. Claim may be rejected for other reasons including Clearinghouse edits or Payer specific validation.
Skipped: During processing the claim was not checked for CCI or MNC. This would happen if the client is not contract for CCI/MNC or if the claim did not have enough data for CCI/MNC validation. Claim may be rejected for other reasons including CH edits or Payer specific validation.
Error: A CCI or MNC error is present. A CCI/MNC error will not reject the claim however the claim may be rejected for other reasons including CH edits or Payer specific validation.
Warning: There is a CCI/MNC related issue. A CCI/MNC warning will not reject the claim however the claim may be rejected for other reasons including CH edits or Payer specific validation.
Error and Warning: There are CCI/MNC related warnings and errors present. Clients have the set up option to not reject claims for CCI/MNC errors. So based on client set-up the claim won't reject for CCI/MNC Errors and Warnings, however the claim may be rejected for other reasons including CH edits or Payer specific validation.
Rejected Error: There is a CCI/MNC error present in the claim. Clients have the set up option to reject claims for CCI/MNC errors. The claim may also be rejected for other reasons including CH edits or Payer specific validation.
Rejected Error and Warning: CCI/MNC errors and warnings are present. Clients have the set up option to reject claims for CCI/MNC errors and warnings. The claim may also be rejected for other reasons including CH edits or Payer specific validation.
CCI
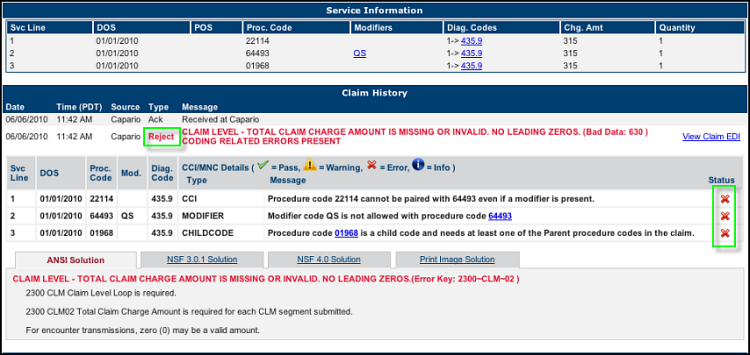
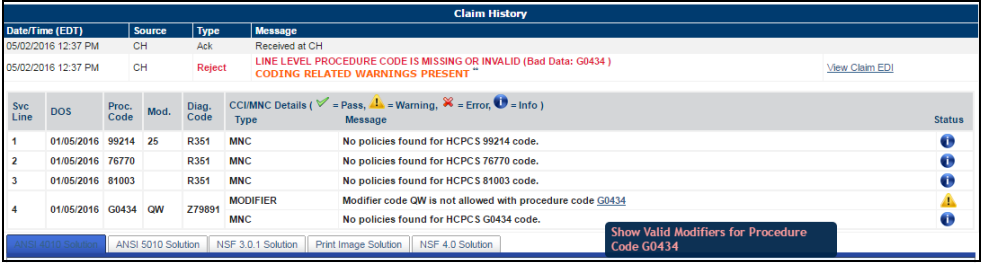
In this example:
The claim was rejected by Clearinghouse and Rejected by CCI.
Result: Claim was rejected.
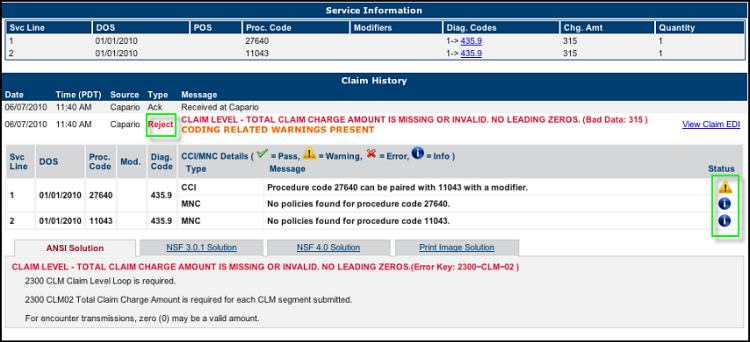
In this example:
This claim was Rejected by Clearinghouse and received a CCI warning.
Result: Claim was rejected.
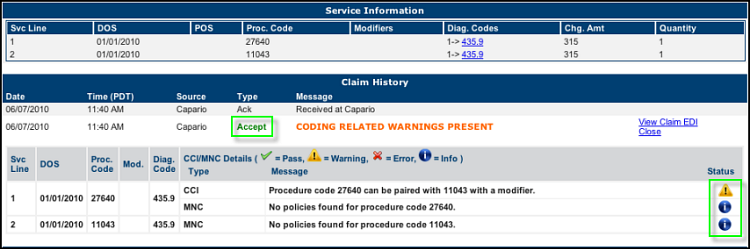
In this example:
This claim was Rejected by Clearinghouse and received a CCI warning.
Result: Claim was accepted.
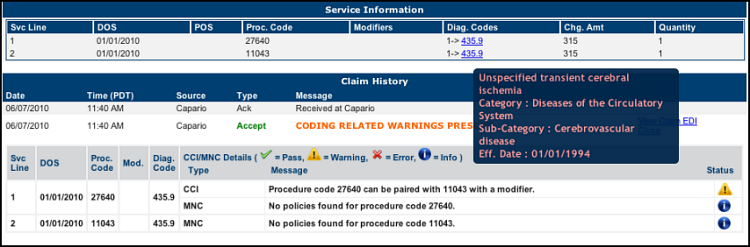
In this example:
Hover over the Diagnosis code to see information.
Click link for more information.
In this example:
This claim shows a CCI rejection.
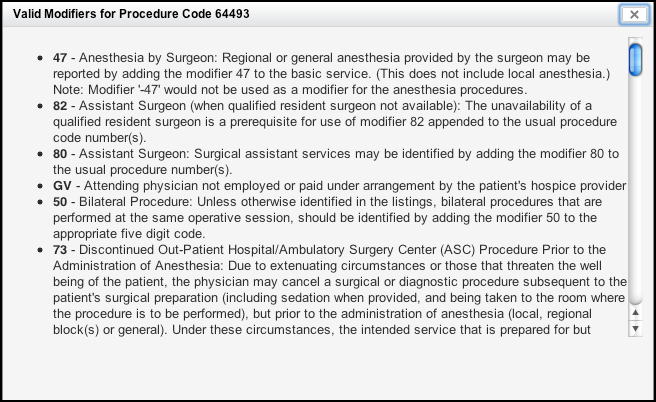
Hover over the procedure code and click to View Valid Modifiers for this procedure code. See next screen.
Below are valid modifiers for this procedure code that can be used to correct the claim.
In this example:
This claim shows a CCI rejection.
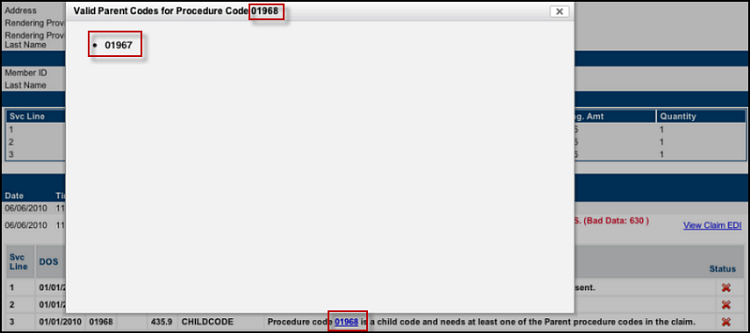
Hover over to view valid parent procedure code. See next screen.
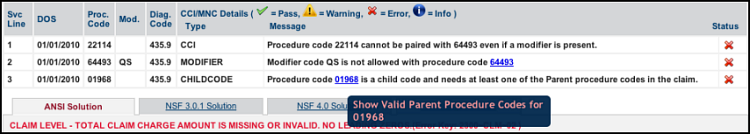
The valid parent code is shown which can be used to correct the claim.
MNC
MNC checks the claim to determine if it can be accepted based on meeting national and local Medical Necessity policies.
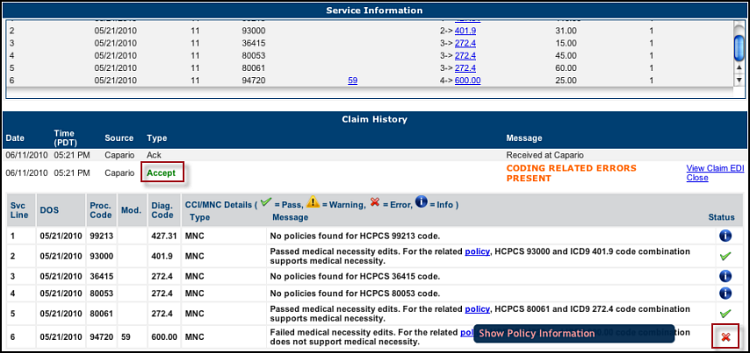
In this example:
TThis claim was accepted by Clearinghouse but rejected based on an MNC check.
Hover to view the policy information that caused the MNC rejection. See next screen.
Policy Information that caused this MNC rejection:
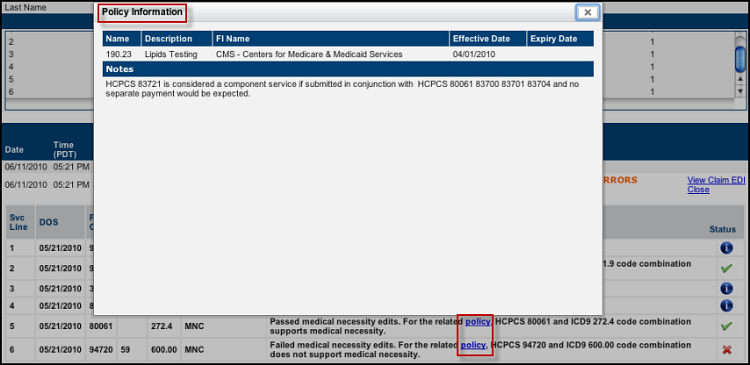
Return to Find Claims help page.